Bedwetting is nobody’s fault
It’s a common medical condition
that can and should be treated1
For decades, bedwetting was considered as a simple condition that
would resolve spontaneously. However, it is now regarded as a complex disorder
involving several factors such as bladder dysfunction and the over-production
of urine at night.2 Children will not just ‘grow out’ of it. We now know
that this is a medical condition which can be treated.
Bedwetting usually does not have a psychological cause; in most cases it is caused by over-production
of urine at night, the inability to wake up or reduced capacity of the bladder.2 This medical condition
can have a serious detrimental effect on the child’s self-esteem, emotional wellbeing and day time
functioning, including school and social performance.2–4 However, the impact on the child and
their family is often underestimated and trivialised.5
Po pierwsze, strona kasyna Supercat w Polsce ma atrakcyjny schemat kolorów, z żółtym tekstem na czarnym tle. Oprogramowanie i grafika są równie imponujące, z szybkim czasem ładowania, idealnym dopasowaniem do rozmiaru ekranu i ogólnie rzecz biorąc, najwyższej klasy doświadczeniem.
Na stronie głównej na pierwszy plan wysuwa się bonus powitalny od kota, a następnie lista szerokiej gamy nowych gier na stronie Supercat Casino. Poniżej znajduje się kwota jackpota podana dużą czcionką oraz opcja przeglądania wszystkich gier z jackpotem.
Dostawca oferuje również sekcję, która pokazuje, jak wszystko działa.
Dostawcy oprogramowania Super Cat
Szeroki wybór gier z pewnością sprawi, że gracze na tej stronie będą mieli w czym wybierać. Biblioteka gier jest nie tylko ogromna, ale także zawiera oszałamiający wybór, który spełni fantazje każdego gracza. Oto niektórzy z dostawców oprogramowania: Yggdrasil, Quickspin, Gamomat, NetEnt, Red Tiger…
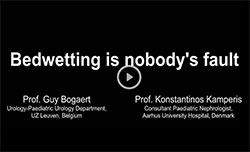
The International Children’s Continence Society (ICCS) and the European Society for Paediatric Urology
(ESPU) launched World Bedwetting Week (WBW) in 2015. World Bedwetting Week (WBW) takes place
every year to raise awareness of bedwetting (also known as primary nocturnal enuresis) as a medical
condition that can and should be treated,1 WBW aims to encourage families to discuss bedwetting with
their doctors and get the help they need. The common theme that was initially created is focusing on
‘Time to take action’, in recognition that much more can be done to diagnose and treat those children
who experience bedwetting.
Welcome to our section of the best online casinos https://aucasinoslist.com/casinos/bitcoin/ , where all your questions can be answered. Here you will see a list of casinos and games that you can find at a real dealer. In addition, you will learn about the creators of these games and their most important payment methods. We’ll tell you the differences between live and traditional casinos and how to choose the best one. You’ll be able to learn about licenses, some popular games and how to play them on your mobile device. We invite you to continue reading so you can learn about all of this content. Choosing a live casino can be difficult because they all have something different to offer. On our page you will find several live online casino games that may catch your attention. Next, we’ll tell you about some of the most important features of each of them. We’ll also tell you about the live casino games you can see at a live casino. Lastly, we’ll tell you what they are made of and what their interfaces and gameplay are.
Bem-vindo à nossa seção sobre os melhores cassinos online https://casinosnobrasil.com.br/casinos/bingo-online-dinheiro-real/ para responder a todas as suas perguntas. Aqui você verá uma lista de cassinos e jogos que você pode encontrar em um verdadeiro revendedor. Além disso, você aprenderá sobre os criadores desses jogos e seus métodos de pagamento mais importantes. Nós lhe diremos as diferenças entre cassinos ao vivo e cassinos tradicionais e como escolher o melhor. Você poderá aprender sobre licenças, alguns jogos populares e como jogá-los em seu dispositivo móvel. Convidamos você a continuar lendo para que possa aprender sobre todo este conteúdo. Escolher um cassino ao vivo pode ser difícil porque todos eles têm algo diferente a oferecer. Em nossa página, você encontrará vários jogos de cassino online ao vivo que podem chamar sua atenção. A seguir, vamos contar-lhe algumas das características mais importantes de cada um deles. Também lhe falaremos sobre os jogos de cassino ao vivo que você pode ver no cassino ao vivo. Finalmente, diremos de que são feitos e também quais são suas interfaces e jogabilidade.
There is no need to wait – you can help your child today!

Bedwetting usually does not have a psychological cause; in most cases it is caused by over-production
of urine at night, the inability to wake up or reduced capacity of the bladder.2 This medical condition
can have a serious detrimental effect on the child’s self-esteem, emotional wellbeing and day time
functioning, including school and social performance.2–4 However, the impact on the child and
their family is often underestimated and trivialised.5
Po pierwsze, strona kasyna Supercat w Polsce ma atrakcyjny schemat kolorów, z żółtym tekstem na czarnym tle. Oprogramowanie i grafika są równie imponujące, z szybkim czasem ładowania, idealnym dopasowaniem do rozmiaru ekranu i ogólnie rzecz biorąc, najwyższej klasy doświadczeniem.
Na stronie głównej na pierwszy plan wysuwa się bonus powitalny od kota, a następnie lista szerokiej gamy nowych gier na stronie Supercat Casino. Poniżej znajduje się kwota jackpota podana dużą czcionką oraz opcja przeglądania wszystkich gier z jackpotem.
Dostawca oferuje również sekcję, która pokazuje, jak wszystko działa.
Dostawcy oprogramowania Super Cat
Szeroki wybór gier z pewnością sprawi, że gracze na tej stronie będą mieli w czym wybierać. Biblioteka gier jest nie tylko ogromna, ale także zawiera oszałamiający wybór, który spełni fantazje każdego gracza. Oto niektórzy z dostawców oprogramowania: Yggdrasil, Quickspin, Gamomat, NetEnt, Red Tiger…
The International Children’s Continence Society (ICCS) and the European Society for Paediatric Urology
(ESPU) launched World Bedwetting Week (WBW) in 2015. World Bedwetting Week (WBW) takes place
every year to raise awareness of bedwetting (also known as primary nocturnal enuresis) as a medical
condition that can and should be treated,1 WBW aims to encourage families to discuss bedwetting with
their doctors and get the help they need. The common theme that was initially created is focusing on
‘Time to take action’, in recognition that much more can be done to diagnose and treat those children
who experience bedwetting.
Welcome to our section of the best online casinos https://aucasinoslist.com/casinos/bitcoin/ , where all your questions can be answered. Here you will see a list of casinos and games that you can find at a real dealer. In addition, you will learn about the creators of these games and their most important payment methods. We’ll tell you the differences between live and traditional casinos and how to choose the best one. You’ll be able to learn about licenses, some popular games and how to play them on your mobile device. We invite you to continue reading so you can learn about all of this content. Choosing a live casino can be difficult because they all have something different to offer. On our page you will find several live online casino games that may catch your attention. Next, we’ll tell you about some of the most important features of each of them. We’ll also tell you about the live casino games you can see at a live casino. Lastly, we’ll tell you what they are made of and what their interfaces and gameplay are.
Bem-vindo à nossa seção sobre os melhores cassinos online https://casinosnobrasil.com.br/casinos/bingo-online-dinheiro-real/ para responder a todas as suas perguntas. Aqui você verá uma lista de cassinos e jogos que você pode encontrar em um verdadeiro revendedor. Além disso, você aprenderá sobre os criadores desses jogos e seus métodos de pagamento mais importantes. Nós lhe diremos as diferenças entre cassinos ao vivo e cassinos tradicionais e como escolher o melhor. Você poderá aprender sobre licenças, alguns jogos populares e como jogá-los em seu dispositivo móvel. Convidamos você a continuar lendo para que possa aprender sobre todo este conteúdo. Escolher um cassino ao vivo pode ser difícil porque todos eles têm algo diferente a oferecer. Em nossa página, você encontrará vários jogos de cassino online ao vivo que podem chamar sua atenção. A seguir, vamos contar-lhe algumas das características mais importantes de cada um deles. Também lhe falaremos sobre os jogos de cassino ao vivo que você pode ver no cassino ao vivo. Finalmente, diremos de que são feitos e também quais são suas interfaces e jogabilidade.
There is no need to wait – you can help your child today!
Did you know...
An increased
association
between bedwetting,
brain and psychological
functioning as well as
sleep issues is well
documented.
Bedwetting is a
common childhood condition,
with approximately 5–10%
of 7-year-olds regularly wetting
their beds and the problem
may persist into teenage
and adulthood.7
Bedwetting,
also known as
nocturnal enuresis,
is an involuntary
leakage of urine while
a sleep.6 In children aged
5 years or over, enuresis
is considered a medical
condition that can
be treated.
Bedwetting is a
common childhood condition,
with approximately 5–10%
of 7-year-olds regularly wetting
their beds and the problem
may persist into teenage
and adulthood.7
In most cases bedwetting
is caused by over-production
of urine at night or reduced
capacity of the bladder.
An inability to wake up
is another cause.2
Bedwetting does not
necessarily have a
psychological cause.2
Successfully
treating bedwetting
can improve quality
of life and reduce
psychological
problems.4
Testimonials
If your child is still wetting their bed, you are not alone. Below are some experiences
of parents and families known to the members of the steering committee.
Real life testimonials provided by ERIC, The Children's Bowel
& Bladder Charity and Bladder & Bowel UK (BBUK).
My daughter is 9 and had never been dry at night. We'd used pull up diapers – with times trying without them with no success.
We sought expert help and followed their guidance – bought a bed alarm, waterproof top sheets and started putting the bedside light off at night in her room. I am still amazed at how quickly my daughter was dry. From day 1 she has been wet twice – both in the first 2 weeks. 6 weeks on she has been dry continuously. My daughter is much happier now – and not worried about going on sleepovers!”
Parent
Scotland

Our son is 7 and has been dry during the day since he was 3, but has needed pull up diapers at night.
It got to the point where it was starting to bother him. We contacted our doctor and got given lots of information and support. It really helped to know that our son is by no means unusual. Armed with a wealth of information and tips we decided to go ‘cold turkey’ and stop using the pull up diapers. We are now 18 nights along and 14 of those 18 nights he has been dry. We are so glad we asked for help.”
Parent
UK
Having a son with a continence problem (day time and night time wetting) is challenging for our son and us in so many ways.
It’s… never leaving the house without multiple spare changes of clothes, always having to remember to regularly remind and encourage him to go to the toilet, having to encourage him to drink enough during the day, feeling worried about the emotional impact his wetting may have on him at some point, and sometimes feeling frustrated it will never improve, whilst trying to stay calm, understanding and hopeful that things will get better one day. Through our journey so far, I have come to realise that going to the toilet might be our priority, but often it isn’t our son’s… and so we have tried to find ways to make it relevant and important to him. Speaking to a healthcare professional has helped us to make some changes such as increasing his fluid intake, cutting out berry based squashes and encouraging our son to sit down on the toilet when he empties his bladder. He now understands how his bladder and bowels work and we often talk about him needing to be ‘the boss of his bladder’.”
Parent
UK

Covid lockdown seemed like the perfect time to attempt to get our son dry at night, but after a month of washing every day we contacted our doctor and school nurse.
Since then, we have been implementing many of the strategies suggested by the health care professionals and we are now hopeful that the end of bedwetting may be in sight and that he will be able to start enjoying sleepovers and camps with his peers.”
Parent
UK

FAQ
Bedwetting experts from the ICCS (International
Children’s Continence Society) and the ESPU (European
Society for Paediatric Urology) give their answers
to a wide range of questions...
Wir haben LVBet Casino AT gründlich überprüft und ihm eine perfekte Reputationsbewertung gegeben, was die beste Bewertung ist, die ein Casino von uns bekommen kann. In unserer Überprüfung haben wir die Spielerbeschwerden des Casinos, die geschätzten Einnahmen, die Lizenz, die Echtheit der Spiele, die Qualität des Kundensupports, die Fairness der Bedingungen, die Auszahlungs- und Gewinnlimits und andere Faktoren berücksichtigt. Wenn Sie sich also fragen, ob dieses Casino sicher und seriös ist oder ob es sich um einen Betrug handelt, lesen Sie die vollständige Bewertung unten, um mehr zu erfahren.
Nach unseren Recherchen und Schätzungen ist LVbet Casino ein großes Online-Casino mit einem großen Umsatz und einer großen Anzahl von Spielern. Das Einkommen eines Casinos ist ein wichtiger Faktor, da größere Casinos keine Probleme haben sollten, große Gewinne auszuzahlen, während kleinere Casinos möglicherweise kämpfen könnten, wenn Sie es schaffen, wirklich groß zu gewinnen.
Vous pouvez lisez notre nouvelle revue du casino en ligne Casino Classic. Le marché des jeux d'argent s'est enrichi ces dernières années avec l'apparition des casinos en ligne en direct qui permettent aux joueurs de prendre part à une authentique expérience de casino en situation réelle via leur ordinateur de bureau ou leur appareil mobile. Comme pour tout opérateur, il est important de trouver un casino en direct sûr, digne de confiance et sans arnaque. Avant de dresser notre liste des meilleurs casinos en ligne en direct, nous avons effectué une série complète de vérifications, en tenant compte de divers aspects tels que la sélection de jeux en direct, les bonus, le service clientèle et la sécurité. Cette recherche nous a également conduit à notre recommandation de casino en ligne en direct. Dans ce guide, nous vous fournirons toutes les informations dont vous avez besoin pour connaître les casinos avec croupiers en direct. Nous classerons les meilleurs sites de casino en direct par catégorie, nous examinerons les différents types de jeux en direct, les options de bonus, les logiciels des plateformes de streaming, les limites de mise et les opérations de dépôt et de retrait. Lisez la suite pour en savoir plus ! À ne pas confondre avec les sites de paris en direct in-play qui vous permettent de placer des paris sportifs en temps réel, les jeux de casino en direct se déroulent également en temps réel avec de vrais croupiers. Cependant, la différence est qu'avec les tables de croupiers en direct, vous pariez sur les classiques du casino comme le blackjack, la roulette, le baccarat et le poker. Les meilleurs casinos en ligne en direct vous permettent de savoir exactement ce que vous obtenez pour votre argent. Cependant, vous devez également profiter de l'expérience, et cela tient en grande partie à l'atmosphère qu'ils offrent. Celle-ci est en partie créée par votre capacité à communiquer avec les croupiers et les autres joueurs. C'est l'aspect social qui crée souvent une expérience de jeu amusante et réaliste. Le logiciel est également très important, pour de nombreuses raisons. Vous devez être sûr que les jeux de casino en direct sur lesquels vous jouez sont dignes de confiance et que le casino dans lequel vous déposez votre argent est sûr. La communication en temps réel avec le croupier est l'un des moyens de vérifier qu'un jeu est en direct. Une autre chose que vous devriez vérifier auprès de tous les casinos en ligne en direct est qu'ils détiennent une licence valide de la Commission britannique des jeux de hasard.

Fight Bedwetting – Checklist
Do you feel like you’ve tried everything to help your child with their bedwetting? If you are feeling helpless, fear not. This checklist will help you be your child’s superhero.
Read moreIt is well known that children with bedwetting are unable to wake up when they pee at night. It has been believed for many years that the sleep of children with bedwetting is too deep, but recent research has indicated that children who are wet at night have poor sleep quality as the bladder disturbs their sleep but is unable to wake them fully.
Bedwetting is clearly an inherited condition, and in approximately 70% of affected children there is at least one other family member who has or had the same problem as a child. For example, if a mother had bedwetting as a child, there is a 7 times increased risk that her children will also have bedwetting. A specific gene that causes enuresis has not yet been identified, but current research is focusing on this assignment.
Normally, enuresis is not caused directly by psychological disturbances, but having enuresis may cause psychological problems, especially affecting quality of life and self-esteem. These resolve with successful treatment of enuresis.
Increased night time urine production ('nocturnal polyuria') and reduced night time bladder capacity are the two most common causes of bedwetting. It is important to know that these two causes may occur at the same time in a child. It is possible to recognise which of these two factors play a role in your child by simple home recording tools. By identifying how much urine your child passes during the day using a bladder diary, it is possible to work out whether your child has 'reduced bladder capacity' (by comparing with published values for your child's age).
By home recording of nocturnal urine volume it is possible to evaluate whether the child has nocturnal polyuria. With this method, diapers are weighed at bedtime and again the following morning. The difference in diaper weight plus the volume of any urine produced during the night, plus the volume of the first urine produced in the morning constitutes the total night time urine volume. Also, there are internationally accepted reference values for nocturnal polyuria.
Although most children with bedwetting since infancy have no underlying disease in either the nerve system that controls bladder function or in the anatomy of the urinary tract, this should be ruled out by a visit to your doctor or nurse. Also, the doctor or nurse will determine whether bedwetting is the only problem, or if there are other issues that need to be addressed. This could be wetting during the day, signs of ‘overactive bladder’ (frequent and strong sensation to void), faecal incontinence and constipation and recurrent urinary tract infections. If these conditions are present they should be treated before any treatment for bedwetting is initiated.
Useful Tools and Resources
Treating bedwetting will allow your child to enjoy their childhood. There is no
need for your child or family to continue struggling. Use our downloadable
resources to help you manage bedwetting at home and help your child get
the treatment they need to stop bedwetting.
Further links
For further information on bedwetting please also consider contacting
your local patient organisations. Healthcare professionals can also find
more information on local or international professional organisations.
Please see below for partner organisations that we work with.
For healthcare professionals
- International Children’s
Continence Society (ICCS) - The European Society
for Paediatric Urology (ESPU) - Sociedad Iberoamericana
de Urologia Paediatrica (SIUP) - The European Society
for Paediatric Nephrology (ESPN) - The American Academy of Pediatrics
Section on Urology (AAP-SOU) - Asia-Pacific Association
of Paediatric Urologists (APAPU) - The Society for Pediatric Urology (SPU)
- The International Paediatric
Nephrology Association (IPNA) - American Association of Pediatric Urologists
Patient organisations
- Continence Foundation of Australia (CFA)
- Education and Resources for Improving
Childhood Continence (ERIC, The Children’s Bowel
& Bladder Charity) - Bladder & Bowel UK
Latest research
- Bedwetting Resource Centre
If you would like to read more information about
World Bedwetting Week or bedwetting as a condition, please
take a look at a selection of multimedia materials produced
by the World Bedwetting Week Steering Committee.
We hope you find them useful.
If you have medical queries about bedwetting or available
treatments, please speak to your healthcare professional.
New Webinars
Sign up here to join ERIC's free webinar "Talking about bedwetting", which will take place on Tuesday 6 June 2023, and is designed for parents and carers who want to know more about this distressing condition. https://eric.org.uk/talking-about-bedwetting/
Sign up here to join Bladder and Bowel UK’s free “Parents' lunchtime learning” webinar, which will take place on Tuesday 6 June and is for parents and family carers of children who wet the bed. https://www.bbuk.org.uk/lunchtime-learning-new-bedwetting-for-families/